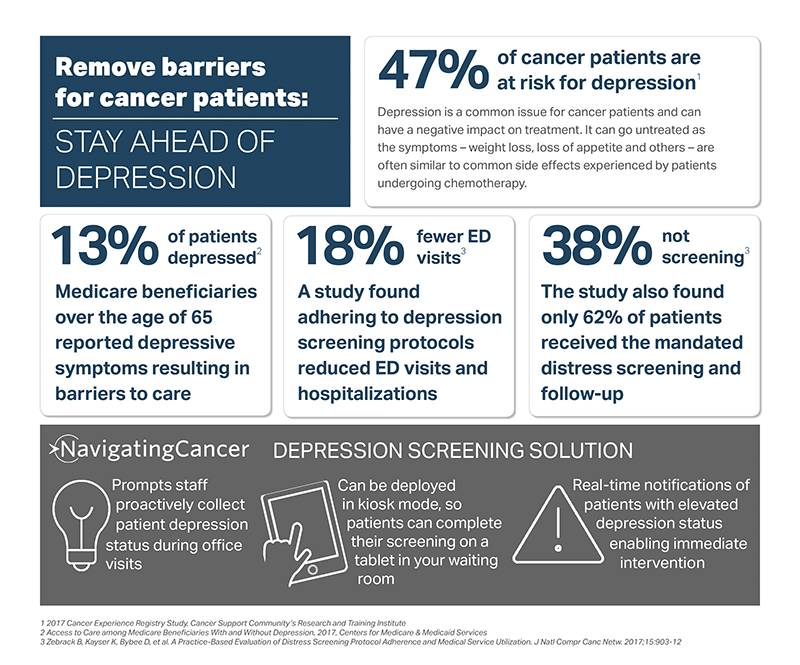
Depression is a common issue for cancer patients and there are obvious reasons for that – the diagnosis itself, uncertainty of the outcome, financial stress and many more. It can also go untreated when the symptoms – weight loss, loss of appetite and others – are often similar to common side effects experienced by patients undergoing chemotherapy.
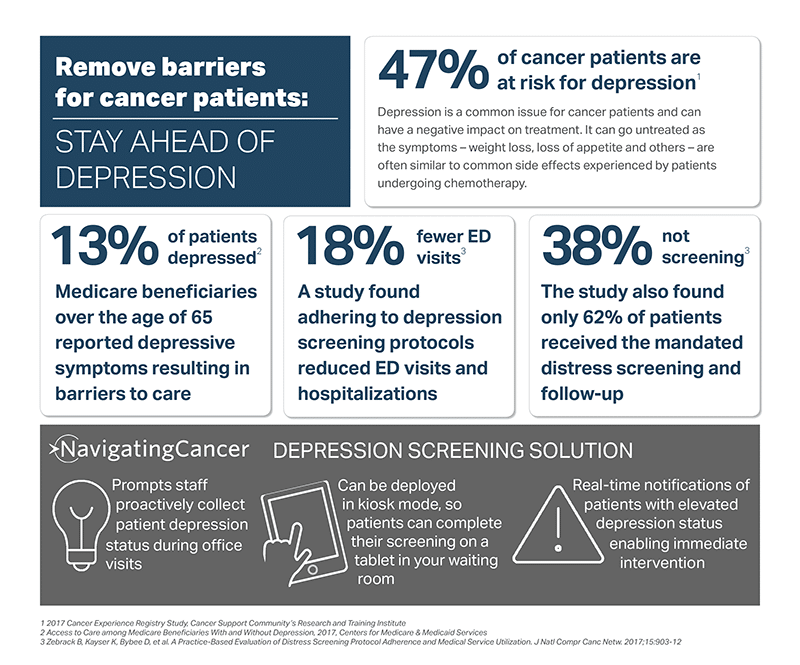
The 2017 Cancer Experience Registry study, developed by the Cancer Support Community’s Research and Training Institute, found that depression is a persistent gap in cancer care – that nearly half (47%) of the 12,000 respondents were identified as at risk for clinically significant levels of depression. And a 2017 survey of Medicare beneficiaries found that depressed people were more likely to report having trouble getting health care, obtaining prescription medicines, and not seeing doctors than those without depression. And for cancer patients, depression can be even more debilitating.
If you’re still not convinced that screening for depression in cancer patients should be a top priority, consider this: a University of Michigan Comprehensive Cancer Center study published this year found that adherence to distress screening protocols set by the Commission on Cancer could lead to 18% fewer ER visits and 19% fewer hospitalizations. The study also found that only 62% of patients received the mandated distress screening and follow-up. Whether the reasons for that are operational or due to a shortage of resources or something else isn’t clear, but they need to be overcome – not only for the patient, but also for the practice as the shift to value-based care continues.
Navigating Cancer’s patient relationship management solution includes depression screening and it can be easily implemented for your patients and staff. It prompts you to proactively collect patient depression status during the office visit and can be deployed in kiosk mode, so patients can complete their screening on a tablet in your waiting room. Your staff receives real-time notifications of patients with elevated depression status so that you can provide immediate intervention and follow up as needed. This information can also be sent back to the EMR so the care team can take into account the patient’s psychosocial well being and factor it into their treatment and ongoing care.
Give patients every tool that can help them adhere to therapy and stay on track.