Advisory Board recently hosted its Oncology Roundtable Virtual Summit with a focus on cancer care after Covid-19. The program started with a question to the audience: “How are you feeling?” Responses included hopeful, proud, overwhelmed, and tired. Clearly cancer care providers have had to face significant challenges and have risen to the occasion to ensure their patients are safe and cared for. With this acknowledgement the presenters then turned to the impact the pandemic has had on healthcare strategy and adoption of telehealth.
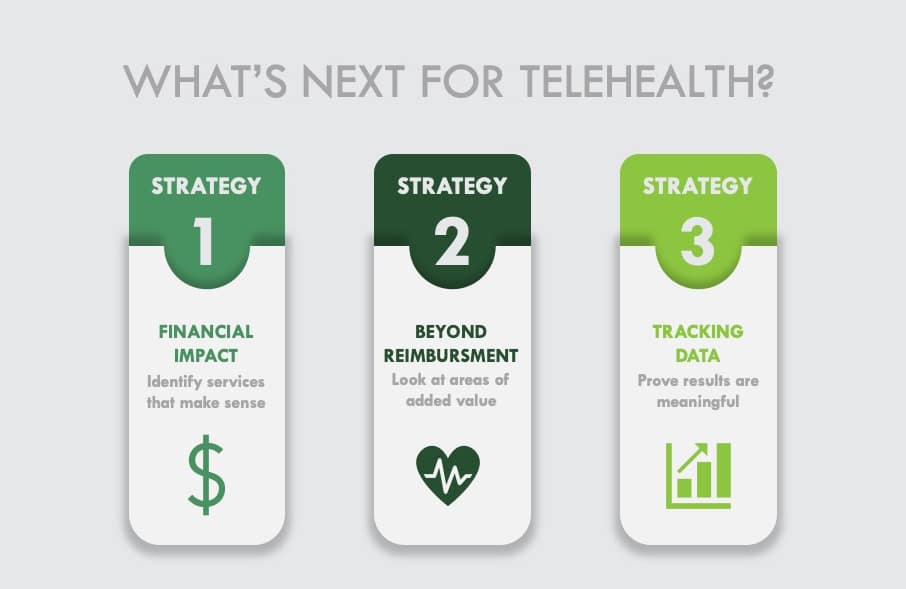
Cancer programs are now facing unprecedented uncertainties and are grappling with how to proceed with capital investments, volume recovery, site of care shifts, and potential restructuring. They also have to think about the future of telehealth and what happens when the Public Health Emergency ends. Advisory Board offered some advice on how to proceed with planning for telehealth offerings:
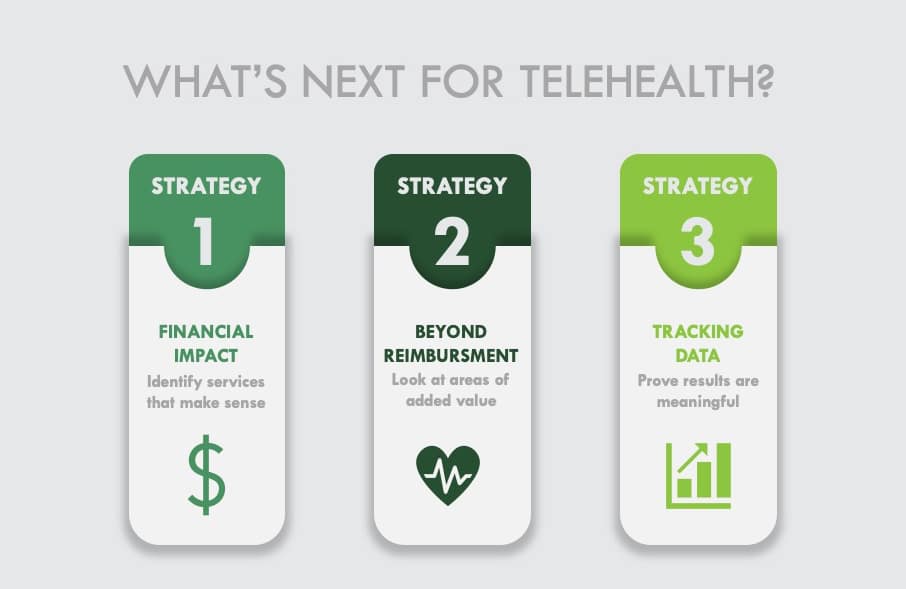
Think about which telehealth services make financial sense
At the expiration of the PHE, there is no guarantee that reimbursement parity to in-person office visits will be sustained for telehealth visits. There are a lot of non-reimbursable services, though, that are appropriate for phone and video based communications including tele-triage, patient education, and symptom management. These support services have a big impact on patient care and patient loyalty as well as ensuring that you stay connected to your patients when they can’t be in the clinic. There are also services that drive downstream revenue like new patient consults where telehealth is a great option since family members can be easily included regardless of their geographic location. And finally, lower revenue services like pre-infusion visits where telehealth is convenient for patients who may live far away, have limited time off of work or mobility issues will help you maintain patient volumes and continue to thrive.
Look for value beyond reimbursement
There are other factors to consider as future reimbursement is unclear for telehealth. It could be an opportunity to increase provider capacity. A subspecialty provider may be able to provide care from one location, but support all of your locations, for instance. Patient loyalty and patient safety are also positively impacted when you can support increased care coordination and minimize patient exposure to the virus.
Use data to identify meaningful value telehealth can offer
Tracking key metrics like rates of readmissions, patient satisfaction, downstream revenue, and increased patient volumes will help you assess the impact of your telehealth services and also prove the value of these services. This will be important moving forward as providers work with payers to increase reimbursement for these important services.
Advisory Board Recommendations
Advisory Board recommends thinking about services that make the most sense to do virtually and eliminate unnecessary in-person visits where you can otherwise maximize patient convenience and safety.
How Navigating Cancer can help
That’s where Navigating Cancer’s patient relationship management digital platform can bridge a lot of the gaps in care in a safe and efficient manner:
- A centralized workboard to track all patient needs by level of urgency
- Triage pathways to standardize and streamline symptom management
- SMS text-based home care instructions to ensure each patient has personalized information directly after a triage incident
- Automated delivery of education that is directly relevant to a patient’s diagnosis and treatment plan
- An electronic patient-reported outcomes system to monitor oral adherence and new or worsening side effects
- Communication tools for cancer programs to easily deliver important information to unique patient populations
- Interested in learning more about our digital health platform?